It’s safe to say Dr. Joanne Ho – an internist, geriatrician and clinical pharmacologist – wears many hats. But the one common thread in her professional life is an interest in medication.
“I found it fascinating how the right combination of medication could make the difference between someone doing really well and not feeling so well and having poorly controlled diseases,” she says of the importance of understanding the impacts of medication when working with older adults.
Dr. Ho completed a mandatory stint at the Ontario Poison Centre during her medical training. “That’s where I saw an amazing interdisciplinary team make a huge difference by providing expertise in poisonings to a large population across a vast geographical area.”
Although the centre housed physicians who specialized in toxicology, Dr. Ho says a majority of phone calls were manned by specialized pharmacists and nurses. Only a fraction required physician involvement.
“Because of the Ontario Poison Centre’s infrastructure and that model of care, they’re able to serve the entire province of Ontario and a few other provinces as well,” explains Dr. Ho. “So it got me thinking, because from a geriatrics perspective, seniors are different. Their bodies change over time and how they process drugs is different.”
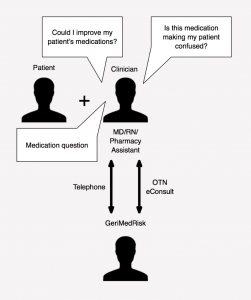
That’s why she created GeriMedRisk, a network of geriatric medication specialists that support clinicians involved in the primary care of older adults. “We’re not an extra prescriber,” Dr. Ho clarifies. “We empower the clinicians that are already involved in the patient’s care.”
GeriMedRisk is currently being tested in long-term care facilities across the Kitchener-Waterloo region, where Dr. Ho and her team are based. The team uses a secure telemedicine platform to connect with clinicians interacting first-hand with older adults.
The CABHI difference
Dr. Ho received financial support from the Baycrest-led Centre for Aging + Brain Health Innovation (CABHI). Our Spark program, which is designed to nurture early stage ideas from point-of-care clinicians, provides up to $50,000 in financial support plus guidance.
“CABHI’s support through the Spark program helped us take off,” says the geriatrician.
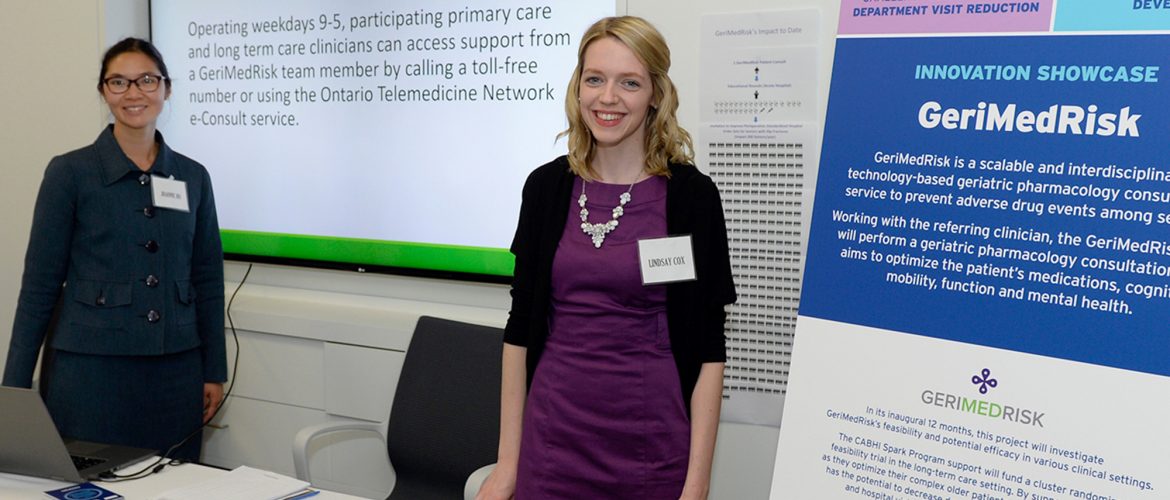
She adds that CABHI fosters a culture of innovation where clinicians such as herself can engage with other innovators. “The innovation showcase that CABHI organized a few months ago was amazing,” says Dr. Ho. “For me, it was truly quite a showcase. It was a great experience just having exposure to so many in
dividuals as well as fellow CABHI projects. From this showcase, I learned to engage with the public, stakeholders, and other groups on a scale that I had never even considered.”
According to Dr. Ho, CABHI has also helped her team think from a business perspective. “It’s important, even as a clinician, for me to be able to speak a different language – the language that administrators and policy makers are speaking. What is a key performance indicator? What are milestones? As a physician, those are unfamiliar concepts. So to be able to learn how to communicate in the same language was a wonderful learning experience.”
The geriatrician is grateful CABHI has maintained and respected her academic freedom and intellectual property. “To receive financial support from an organization like CABHI and to know that they support our research and respect that it’s still our research carries weight. We are very appreciative of CABHI’s support.”
Feasibility trial
CABHI’s support is helping Dr. Ho conduct a feasibility trial for GeriMedRisk. The team conducted a needs assessment with more than 70 clinicians in the Waterloo-Wellington region and is currently trialling its service in four long-term care facilities. “What we do is we randomize the order that four long-term care sites would start to get access to GeriMedRisk.”
Dr. Ho and her team are midway through the trial and so far the results are quite positive. “It also validates the fact that we are empowering the existing circle of care, the existing team members, as opposed to inserting ourselves as additional prescribers. There are a lot of excellent well-staffed, high functioning clinicians and teams who provide great care to their seniors. And we want to support them if they would like additional support managing their older adult patient’s medications, chronic diseases and/or mental health.”
One primary care physician who works in a long-term care setting said the following: “[GeriMedRisk] is an excellent example of collaborative care. It is extremely valuable in my eyes – totally helpful! [The] family [was] happy with the care and outcome.”
In addition to positive feedback from clinicians, her team has also received reassuring comments from older adults. One long-term care resident shared that “without the [GeriMedRisk] recommendation I would still be on too many medications … It’s a great service and I would recommend it highly to anybody”.
Dr. Ho adds that her innovation was conceived in a relatively small city as opposed to a large urban centre. CABHI has been instrumental in helping her team move the project forward.
“It’s the support from large organizations, like CABHI, that allowed this project to become what it is now. We’re at an exciting time of growth and it’s happened quickly, and with the right team. I have to say a big thank you to CABHI.”
- A visual representation of what GeriMedRisk does. Click to expand.